
A recent Washington Post opinion piece spotlighted a growing crisis: mobility decline in older adults — especially those in nursing homes — is accelerating costs, hospitalizations, and loss of independence.
But here’s the uncomfortable truth:
Falls don’t start with the fall.
They start with subtle changes in gait and endurance.
Slower steps.
Shorter strides.
More variability.
Earlier fatigue.
The body whispers long before it screams.
And yet we still don’t treat mobility like a vital sign.
We should.
Because every step tells a story.
“A facility can receive high marks for preventing falls while presiding over widespread mobility loss. Safety becomes defined as keeping people still.” - Washington Post “The Vital Measure of Senior Health that Medicare Ignores” February, 2026
Following a 2025 independent analysis of data captured from more than 500 skilled nursing, assisted living, and independent living communities, OneStep’s outcomes data shows something powerful:
85–90% of patients remained stable or improved
In AL/IL settings, where expected decline is common, stability is not neutral — it’s success. Maintaining function means preserving independence, quality of life, and dignity.
When gait and endurance are measured consistently, decline is no longer invisible.
It becomes actionable.
The Washington Post article emphasizes the financial burden of mobility decline. Our data quantifies it.
500 facilities using OneStep experienced:
That’s not just cost savings.
That’s avoided hospital transfers.
Lower liability exposure.
Stronger quality metrics.
And most importantly — fewer residents experiencing trauma.
Fall prevention isn’t about reacting better.
It’s about seeing risk earlier.
“Medicare mandates assessment of whether residents can walk 50 feet, stand from a chair, move from bed to bathroom independently. These measures are publicly reported, but they rarely trigger the kind of investigation, corrective action or enforcement that follows a fall or an infection.” - Washington Post “The Vital Measure of Senior Health that Medicare Ignores” February, 2026
A resident may pass a short hallway test. But what happens after five minutes? Ten?
Endurance decline often shows up before catastrophic events:
If we only measure snapshots, we miss the trend.
When mobility is monitored continuously — in real life, not just in a clinic — we see who is declining, who is plateauing, and who is quietly improving.
We are how we move.
Historically, gait analysis required labs, wearables, and specialized equipment.
OneStep changed that.
With just a smartphone in a patient’s pocket:
No calibration.
No extra hardware.
No workflow disruption.
When assessment becomes simple, it becomes scalable.
And when it becomes scalable, it becomes preventive.
Mobility as a vital sign doesn’t just improve clinical outcomes. It transforms operations.
From our 2025 analysis of over 500 facilities:
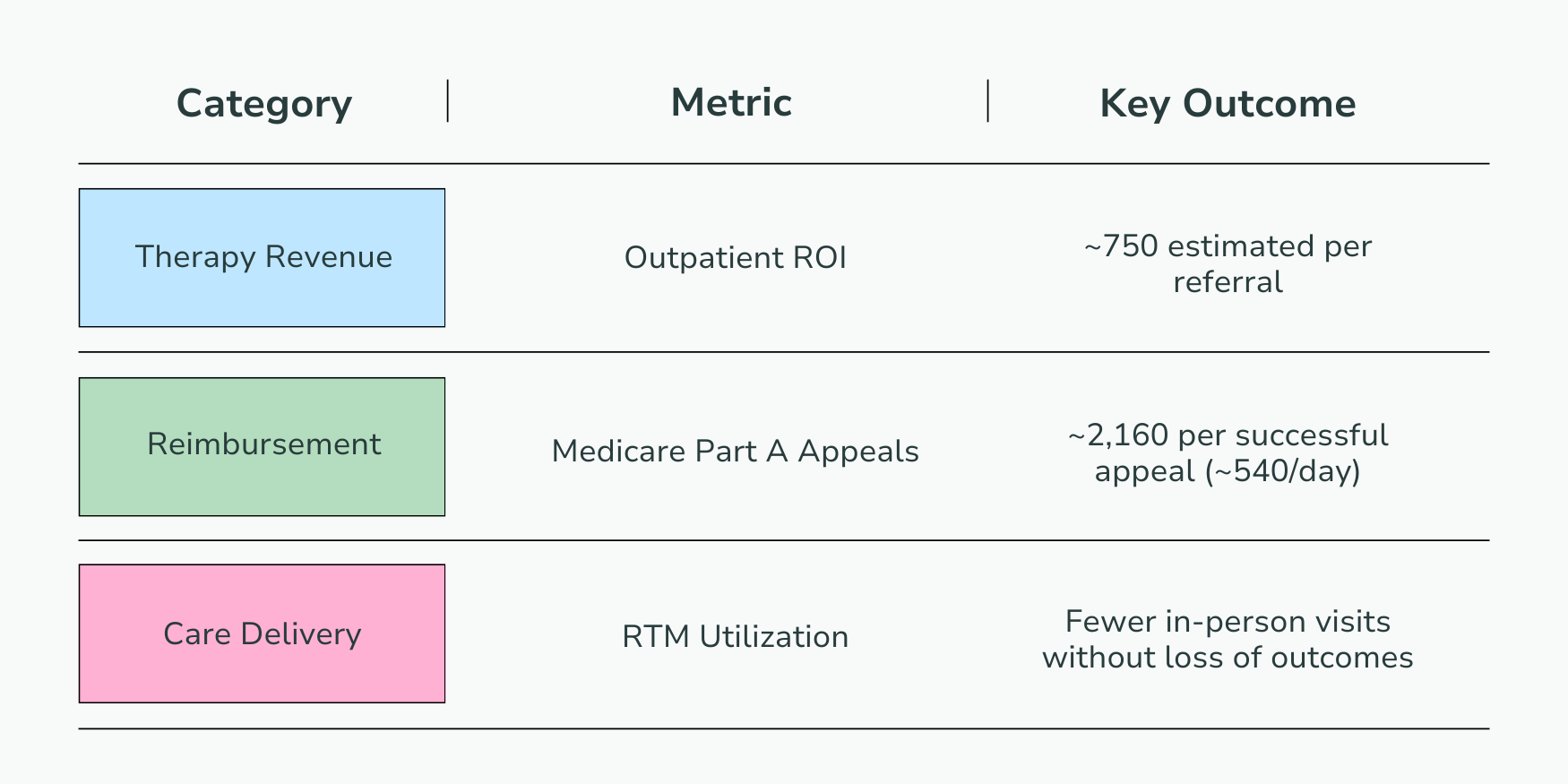
Facilities also unlocked:
Mobility data reduces uncertainty around discharge timing, supports safer transitions, and drives confident clinical decisions.
When you measure movement consistently, you reduce guesswork everywhere else.
The Washington Post article calls for systemic change in how we approach mobility in seniors.
Here’s the OneStep shift:
Instead of asking, “Why did they fall?”
We ask, “What changed in their gait last month?”
Instead of waiting for hospitalization,
we intervene when endurance trends downward.
Instead of subjective impressions,
we use objective, real-world data.
Because when healthcare moves forward at the level of the simple step, just about anything is possible.
Imagine if every intake included a 30-second walk.
If quarterly screenings flagged decline automatically.
If discharge timing was guided by continuous mobility data.
If families could see objective stability — not just hear reassurance.
This isn’t theoretical.
It’s already happening across hundreds of communities.
Every step tells a story.
The question isn’t whether gait and endurance matter.
The question is why they aren’t monitored with the same rigor as blood pressure. It’s time to make mobility a vital sign.
Mobility is becoming one of the most important trends in healthcare.
See how leading organizations are turning movement into measurable prevention:
👉 Movement is more than a moment.
Because we are how we move.