
Gait is now called the 6th vital sign, and for good reason. There’s much to learn from the way a person walks and changes in gait can be an indication of an underlying condition impacting mobility. Monitoring gait in a patient’s natural environment offers a window into how they move during real-life circumstances over a period of time, providing important context that is lacking in traditional care models.
Using remote gait and motion analysis technology to monitor patient mobility enables providers to better understand their patients and tailor interventions when it’s needed the most.
A 67-year-old female patient diagnosed with spondylolisthesis and bilateral hip and knee osteoarthritis was receiving physical therapy services in her home. Her goals were to improve her gait and strengthen her muscles so she could feel more independent and improve her quality of life. At the end of treatment on August 5th, 2022, the clinician decided to transition her to a remote care program. This enabled the extension of the patient's period of care, ongoing engagement in her home program, and continuous monitoring of her gait and progress to intervene in real time. Remote care programs using OneStep are also fully covered by the new Remote Therapeutic Monitoring (RTM) codes.
The OneStep app enabled her physical therapist (PT) to continue to follow her progress, stay in touch, and receive notifications of any changes in her patient data.
The patient was highly engaged using the OneStep app and showed continued improvements. OneStep captured 583 patient walks and 52/56 active days. However, the week of August 15th the patient’s data began to indicate reduced engagement in her home exercise program, a decline in her gait metrics, and a drop in her Patient Specific Functional Scale scores. OneStep’s technology picked up on these changing trends fast and notified the patient’s PT. The PT was able to review the patient’s data in detail and even see exactly which gait parameters were showing unfavorable trends.
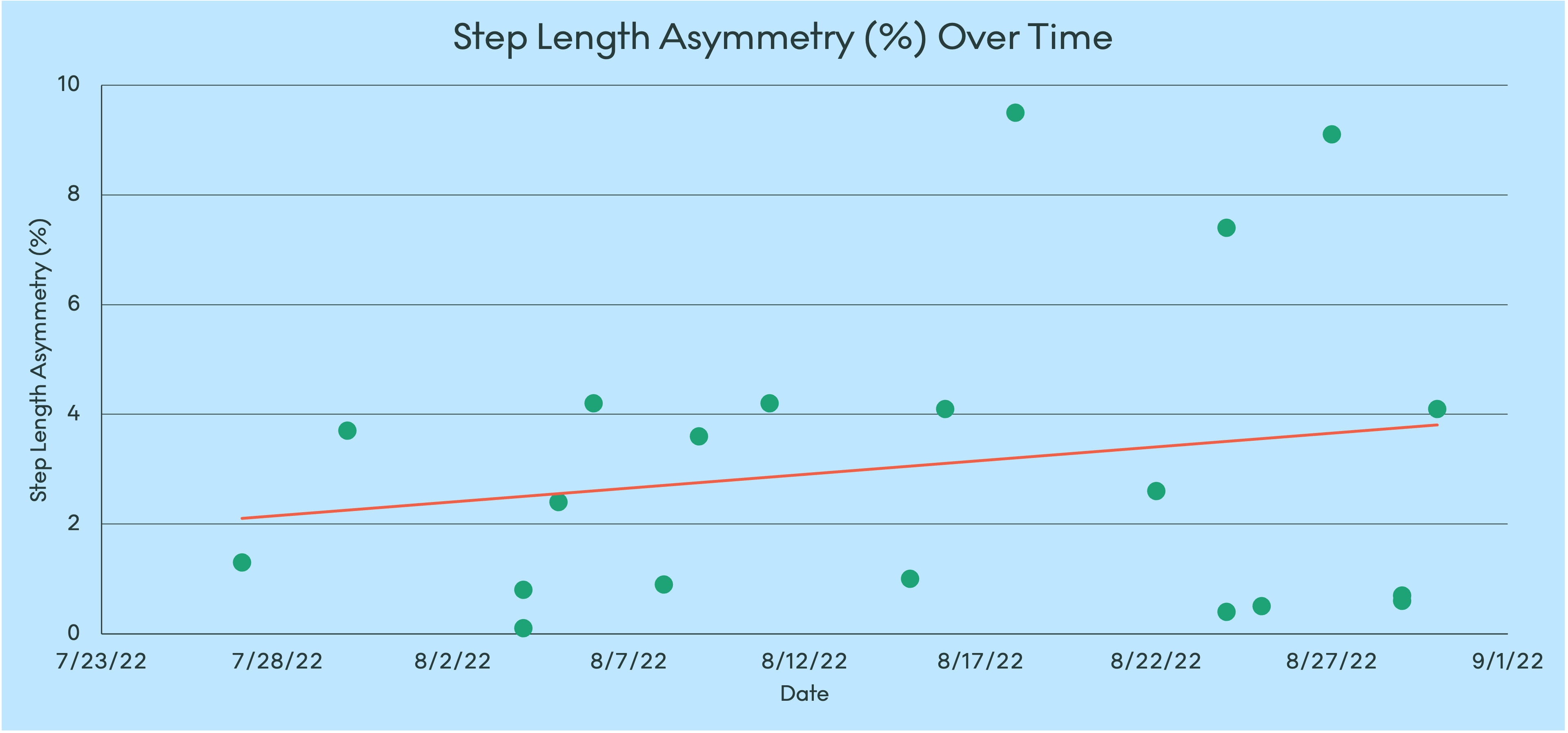
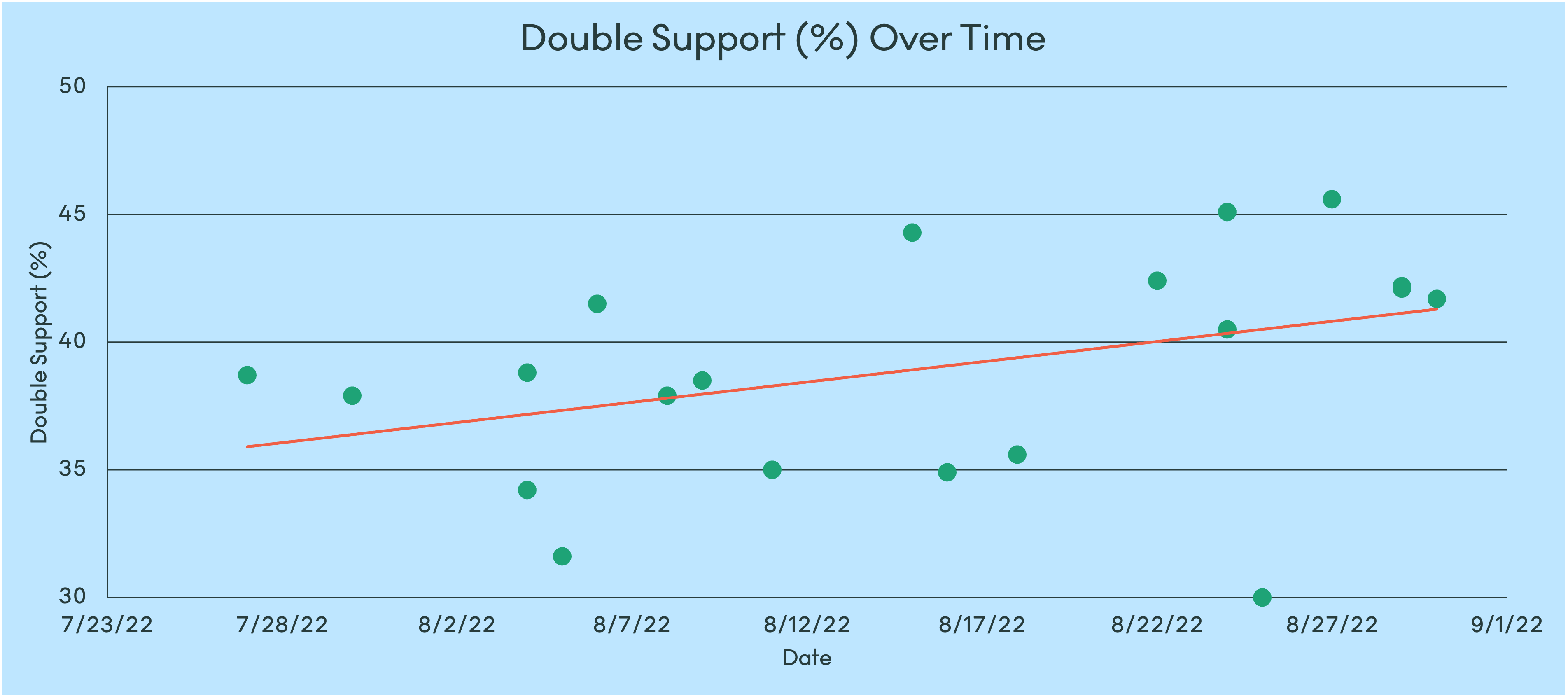
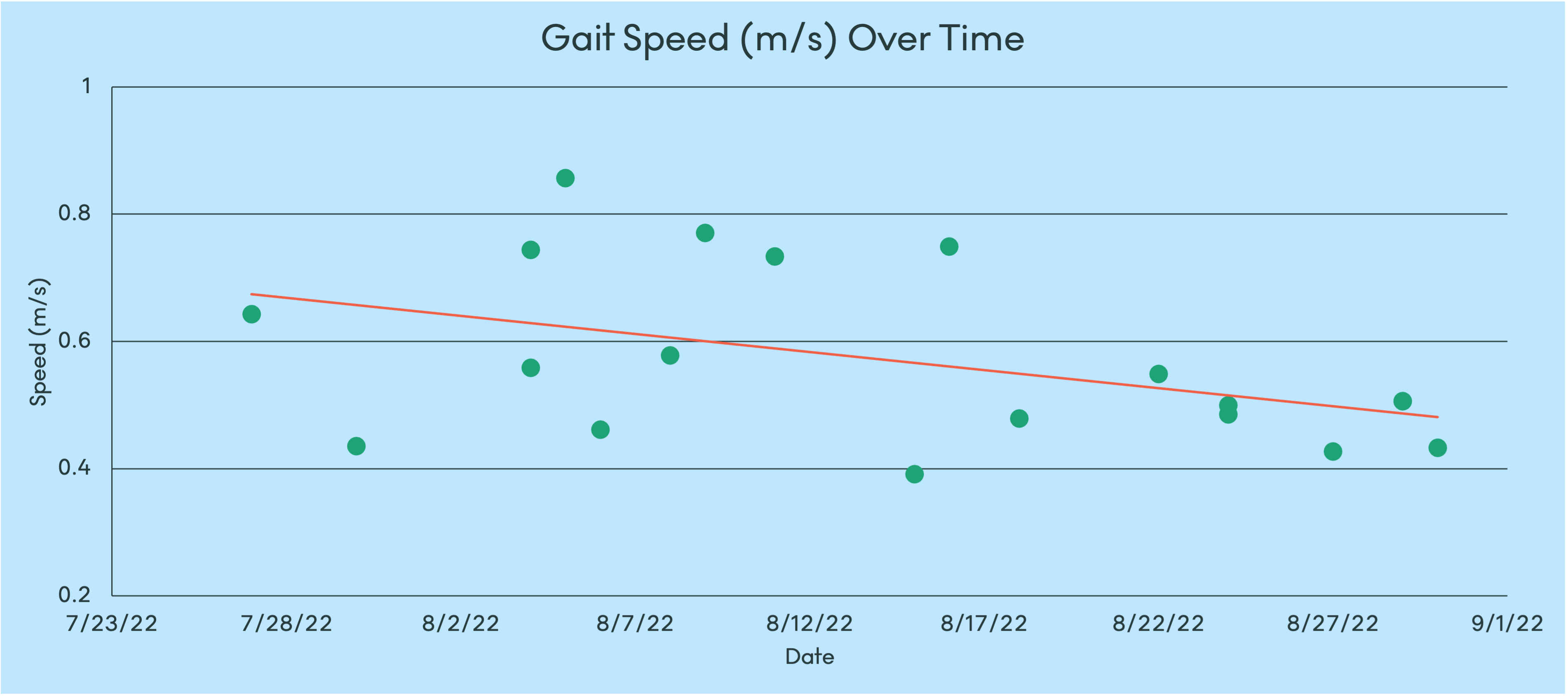
The patient had also been regularly completing the Patient Specific Functional Scale (PSFS) within the OneStep app. The PT could see that her scores started to decline, dropping from 8.3/10 to 3/10. This indicated a significant change and also meant both the patient’s objective gait metrics and self-reported measures were trending unfavorably over the same time span.
.png)
With the automatic notifications and access to such thorough patient data, the PT quickly realized something was amiss with this patient – and determined she needed a follow-up.
The PT reached out to the patient via a telehealth visit and discovered she had recently lost a close friend. The patient confided in the PT that she had not been feeling herself lately and was struggling with grief and depression. Knowing this, the PT was able to provide the patient with the resources she needed and tailor her plan of care to get her back on track toward her mobility goals, while being mindful of this sensitive time in her life.
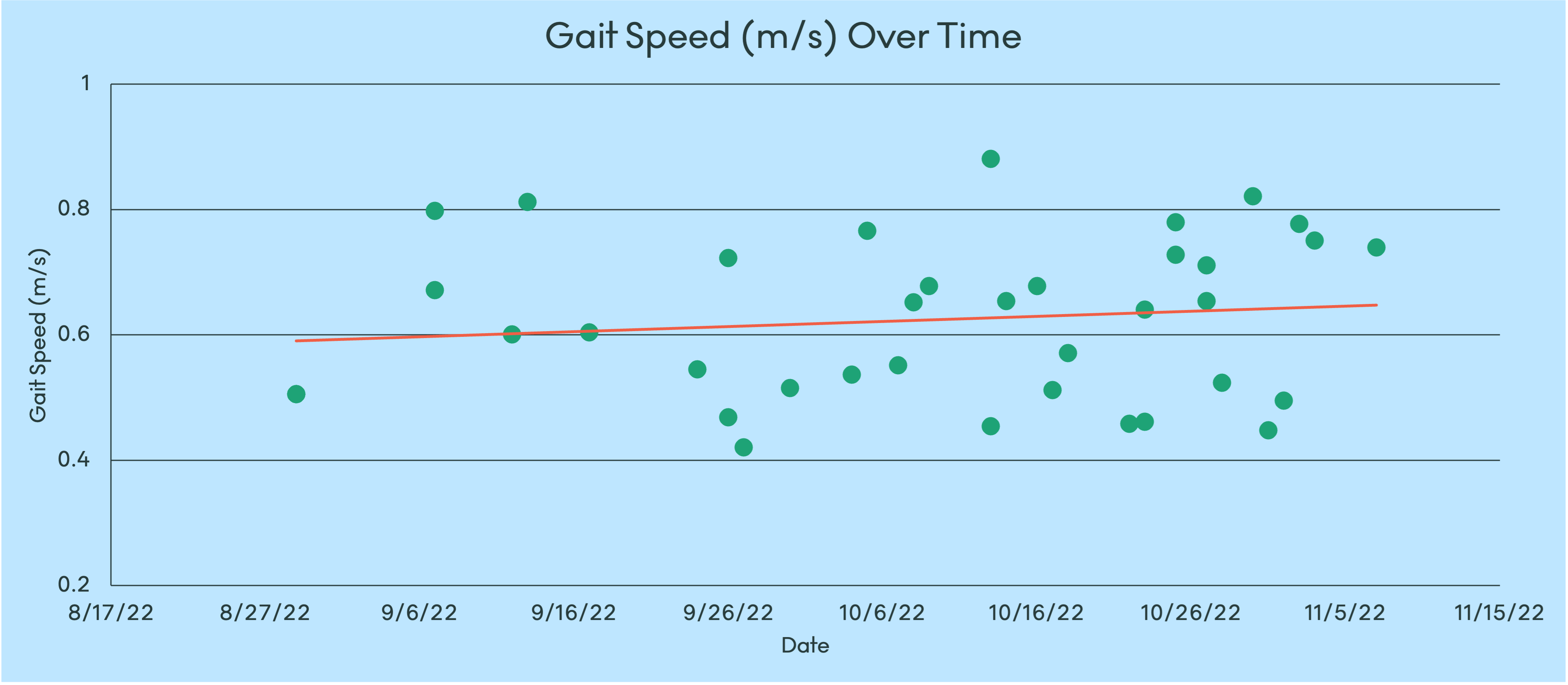
Without OneStep’s technology, the patient may have continued to decline without ever receiving the care she needed – an unfortunate scenario that happens too frequently in traditional care models. With unprecedented insight into the patient’s everyday mobility and seamless communication channels, the PT was able to not only identify the need for intervention but also act immediately. The key to personalized care is to truly understand the patient from a holistic viewpoint, which can be challenging to do under the time and resource constraints of typical practice. RTM with OneStep allows care to transcend in-person visits using data-driven solutions, strengthening the therapeutic alliance for meaningful patient outcomes.